The Department of ObGyn celebrates World Menopause Day with Dr. Susan Reed
 Today, October 18th, is World Menopause Day. To celebrate, we spoke with Dr. Susan Reed, Professor and Vice Chair of Research in the Department of Obstetrics & Gynecology. Dr. Reed provided insight on current menopause symptom management options and her career-long research into menopause interventions.
Today, October 18th, is World Menopause Day. To celebrate, we spoke with Dr. Susan Reed, Professor and Vice Chair of Research in the Department of Obstetrics & Gynecology. Dr. Reed provided insight on current menopause symptom management options and her career-long research into menopause interventions.
Tell me about your research relating to menopause!
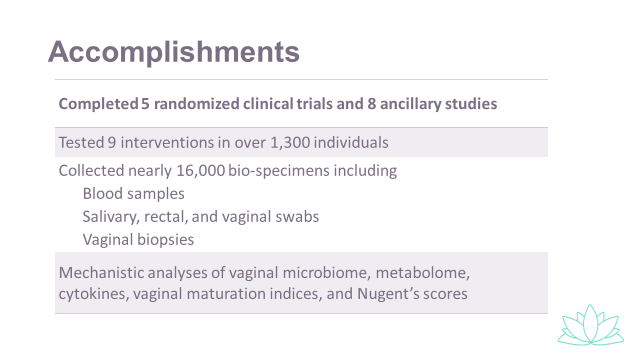
I have been one of 3 MPI of the only clinical trials network for menopause ever funded by NIH, the MsFLASH clinical trials network with my colleagues Dr. Guthrie and Dr. LaCroix. We received funding for nearly 15 years. We had research sites and collaborators at Massachusetts General Hospital, University of Pennsylvania, University of Minnesota, University of Indiana, Kaiser Permanente Oakland Medical Center, University of California San Diego, University of Chicago, and University of California San Francisco. Our clinical site in Seattle was at Kaiser Permanente Washington and the data coordinating center was at Fred Hutch.
Why did you choose to research menopause?
When I was in private practice, prior to coming to UW in 1997, I had many patients taking black cohosh with no evidence demonstrating benefit. With my colleague Katherine Newton, at GHC, now KPWA, and a colleague at Bastyr, Jane Guiltinan, we wrote an NIH R01 that was funded to perform an RCT to evaluate:
- Black Cohosh
- A multibotanical containing black cohosh with a soy diet
- Conjugated equine estrogen
All of these were compared with a placebo.
We found no benefit of the herbal or diet therapies over placebo in this 52 week trial. Only the gold standard arm, estrogen, demonstrated the expected benefit of a decrease in hot flashes by about 80%. Multiple observational studies and clinical trials have followed.
In your opinion, what have been the most impactful findings of your menopause research and why?
With the release of findings from the Women’s Health Initiative, demonstrating a small but real increased health risk with hormone therapy for women over age 60, our patients asked for more nonhormonal therapies. The press sensationalized all negative findings from the WHI and it has been a long battle back to a more balanced approach to caring for our patients with menopausal symptoms.
First, our team published a seminal paper on a head to head comparison of low dose venlafaxine and low dose estrogen for hot flashes and found both medications decreased hot flashes by about 50%; whereas placebo decreased hot flashes by about 30%. Standard doses of hormone therapy decrease hot flashes by about 80%. This information gives our patients important information when they choose a therapy.
Second, we studied CBTI for menopause related sleep disturbance and found it to be more beneficial than low dose estrogen, exercise, yoga, or 2 nonhormonal medications, for hot flashes, escitalopram and venlafaxine.
Third, we found 50% reductions in hot flashes with a low dose antidepressant, escitalopram, as compared with placebo with a 30% reduction. Escitalopram has an excellent safety and side effect profile. This study established a new nonhormonal therapy for women with breast cancer and menopausal symptoms.
Fourth, we studied yoga (weekly classes and practice developed for menopause) and exercise (tailored to the participant and guided in an exercise physiology research center) and found no benefit of these interventions, using a creative study design called 3 x 2 design that provides control groups and minimizes bias.
Last, we evaluated the benefits of vaginal estrogen vs a moisturizer vs control in our vaginal health study. We saw no benefit of the vaginal estrogen or the moisturizer over the control group demonstrating the etiology of postmenopausal symptoms is complex. Evaluation of the vaginal microbiome was not correlated with symptom relief.
Are there any articles relating to menopause that you would like people to read?
Our team's paper "Lights on MsFLASH: a review of contributions", discusses all findings from the MsFLASH trial!